Insulin resistance explained
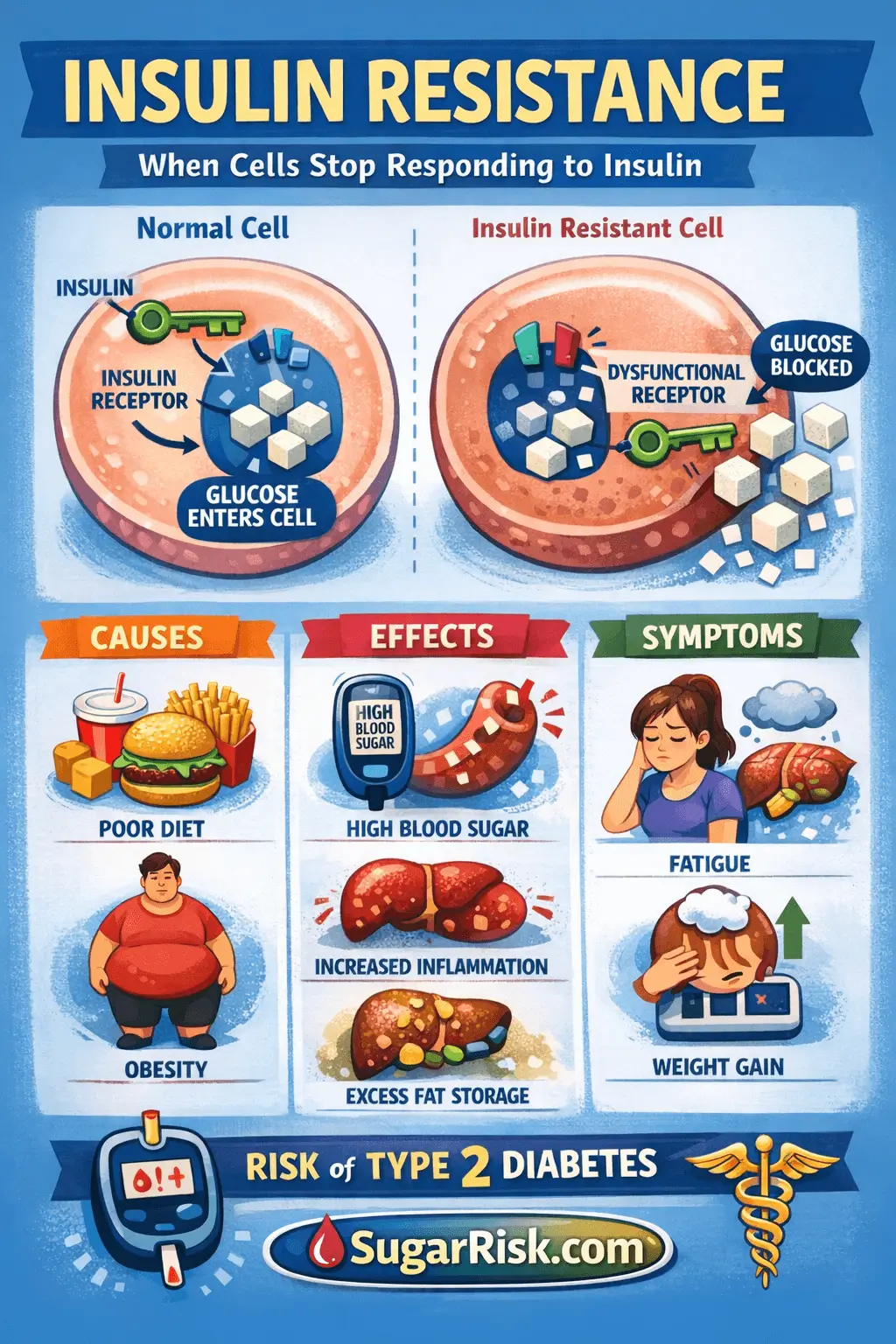
Insulin resistance means your cells do not respond to insulin as well as they should. The body has to produce more insulin to keep glucose in range. Over time, this extra effort can fail, leading to prediabetes and type 2 diabetes.
What insulin normally does
Insulin is a hormone made by the pancreas. After you eat, blood sugar rises and insulin acts like a key, helping glucose move from the blood into cells, especially muscle and fat cells, where it can be used or stored.
In a person with normal insulin sensitivity:
- Blood sugar rises after a meal.
- The pancreas releases a modest amount of insulin.
- Cells respond quickly, take up glucose and levels fall back.
What changes in insulin resistance
In insulin resistance, cells become less responsive to insulin. The same amount of hormone has a weaker effect, so the pancreas has to produce more:
- Insulin levels go up and stay higher for longer.
- Glucose may stay slightly elevated after meals.
- Over time, fasting glucose and A1C can drift upward.
For a while, the body compensates. You can have high insulin and still “normal” glucose on blood tests. This silent phase can last years before prediabetes appears.
Where insulin resistance shows up in the body
Insulin resistance is not just about blood sugar – several organs are involved:
- Muscle – uses less glucose after meals, so more stays in the bloodstream.
- Liver – may keep releasing glucose even when levels are already high, especially overnight and early morning.
- Fat tissue – stores more fat around the organs and waist, and releases substances that can worsen inflammation.
Why some people develop insulin resistance
Common contributors include:
- Genetics and family history of type 2 diabetes.
- Higher body weight, especially central/abdominal fat.
- Low daily activity and long sitting time.
- Highly processed, high-sugar, high-calorie diets.
- Chronic stress and poor sleep.
- Hormonal conditions such as PCOS or some thyroid disorders.
Not everyone with insulin resistance is overweight. Some people at a “normal” weight may still have high visceral fat or genetic risk.
How insulin resistance relates to prediabetes
Prediabetes is often the point where the pancreas can no longer fully compensate for insulin resistance:
- Insulin resistance has been present for some time.
- Insulin levels are high, but not high enough to keep glucose normal.
- Fasting glucose, A1C or OGTT results move into the prediabetes band.
This stage is a critical window. Lifestyle change and, in some cases, medication can reduce the chance of progressing to type 2 diabetes.
Metabolic “cluster”: blood pressure, lipids and liver
Insulin resistance rarely travels alone. Many people also have:
- Higher blood pressure.
- Raised triglycerides and lower HDL (“good”) cholesterol.
- Fatty liver (non-alcoholic fatty liver disease, NAFLD).
This combination is sometimes called metabolic syndrome and is strongly linked to long-term cardiovascular risk as well as diabetes risk.
How SugarRisk approximates insulin resistance
The SugarRisk index does not measure insulin directly, but it uses several factors that tend to move together with insulin resistance:
- Body mass index (BMI) and waist circumference.
- Activity level and sitting time.
- Blood pressure and family history.
- Fasting glucose and A1C if you enter them.
- Optional lifestyle factors such as sugary drinks, smoking and sleep.
A higher index often reflects a higher probability of underlying insulin resistance, even before formal lab tests confirm it.
What you can discuss with your doctor
If you suspect insulin resistance, you can ask about:
- Checking fasting glucose, A1C and a basic lipid panel.
- Whether weight, waist or blood pressure are in a safe range for you.
- Signs of fatty liver on blood tests or imaging, if relevant.
- Whether structured lifestyle programs or medication are appropriate.
Link with your SugarRisk index
A higher SugarRisk index does not prove insulin resistance, but it often points to the same risk cluster. Over months, you can use the index as one of several tools to track progress as habits and lab values change.
Where to go next
Continue learning: What is prediabetes? → or try the SugarRisk calculator →